According to statistics, this disease develops in women more often than in men. These veins appear in the legs and become more common with age.
Further in the article are listed important facts about varicose veins, relevant photos are given to better understand what they look like, what they are and how to treat them.

What are varicose veins?
Varicose veins are abnormally enlarged veins that usually develop in the legs. Typically blue, purple or leather.Looks like enlarged, twisted and swollen blood vessels that may protrude above the surface of the skin.
What are spider veins?
Spider veins (also called telangiectasias or spider veins, vasculature) are a collection of small blood vessels that develop near the surface of the skin.
They are often red, blue or purple and have a grid-like appearance. The most common spider veins are found on the face and legs.
What causes the development of varicose veins?
Varicose veins are caused by structural abnormalities in the blood vessels.Veins carry blood from different parts of the body back to the heart. They have a series of one-way valves to prevent blood flow.
For a variety of reasons, these valves can be damaged, causing blood to flow back into the veins. Further stagnation of blood increases the pressure inside the vein and weakens the vessel wall.
Then, due to blood clots and dilation of the affected blood vessels, arachnoid and varicose veins develop.

Reasons for development?
There are many different risk factors that increase a person's chances of developing varicose veins.
These include:
- old age,
- prolonged standing or sitting,
- mbipesha,
- pregnancy,
- hormone therapy,
- taking birth control pills,
- damage,
- anterior vein surgery,
- history of venous thrombosis,
- family history.
Symptoms of varicose veins
Varicose veins often show no symptoms or signs other than their undesirable cosmetic appearance. However, some people may experience certain symptoms from varicose veins.Symptoms may include:
- edema,
- pulsating sensation
- pain,
- burning sensation,
- itching,
- severity,
- tingling or leg cramps.
These symptoms often worsen after sitting or prolonged standing. Individuals may also develop brown skin and eventually trophic ulcers.
Complications of varicose veinsIf varicose veins are not treated, this can lead to the following:
- Trophic skin ulcers develop. These open sores usually appear on the lower part of the foot. Sometimes they can lead to the development of a soft tissue infection.
- Blood clots develop inside the veins (superficial thrombophlebitis).
- Possible bleeding from the veins.

Diagnosis of vascular network and varicose veins of the legs
To diagnose the presence of varicose veins in the legs, you can carefully examine the affected area, which is usually the foot.
Examination consists of a visual examination and touch of the problem area. Particular attention is paid to areas of redness, swelling, skin discoloration and trophic ulcers.
Home treatment
There are various methods that you can apply at home to help relieve some of your symptoms if they occur. These conservative methods can also help prevent any possible complications.
Compression stockings
Compression stockings are a simple home treatment measure to help relieve foot symptoms.
They improve blood circulation by increasing pressure on the legs. These socks come in different types and hardness in printing. Your doctor may recommend a suitable pair for you. Usually sold in pharmacies.

Lifestyle changes
A regular exercise and weight loss program can help relieve the symptoms of arachnids and varicose veins.
Affected people should avoid standing or sitting for long periods and raising their legs while sitting or sleeping to improve circulation and reduce swelling of the feet.
Scleotherapy
Sometimes conservative treatment of varicose veins at home may not give the desired results. In these cases, more specialized medical procedures may be performed, depending on the location and size of the abnormal veins.
These medical procedures are often performed for cosmetic reasons.
Scleotherapy is a common technique that can be performed by a doctor; is very effective in eliminating most spider veins and some varicose veins.
During this procedure, which does not require anesthesia, the doctor injects a liquid solution directly into the affected vein, causing it to stick together and eventually disappear. Multiple sessions may be required to achieve optimal results. Possible side effects include bruising, swelling, bleeding, infection and skin blemish.
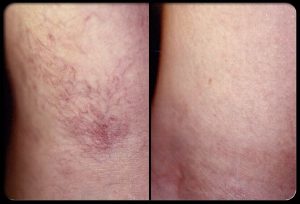
Scleotherapy: before and after
Sclerotherapy treatments can require many sessions and the healing time can vary from person to person.
Generally, spider veins begin to disappear within 3-6 weeks after treatment, while varicose veins may take several months to heal.
Laser treatment of varicose veins
Laser therapy is another alternative medical procedure that a doctor can also perform. Sometimes used in addition to sclerotherapy to maximize results. This technique is most effective for spider veins and veins with small varicose veins.
For those patients who are afraid of needles, laser therapy offers an alternative treatment option, although a doctor may advise you on which treatment is best for your particular situation.
Laser therapy uses a concentrated beam of light that heats the affected blood vessel, which eventually disappears.
Possible side effects include slight redness or swelling around the treated area, skin blemishes, blisters, and rarely scarring.
Laser therapy is a recently developed treatment for varicose veins, in which the affected area is treated with light pulses of different ranges.
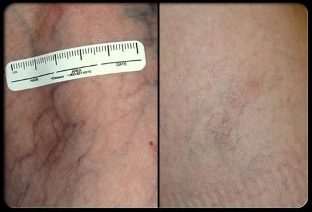
Laser therapy: before and after the procedure
As with sclerotherapy, multiple laser sessions are often required to achieve optimal results. Improvement can take several weeks to several months after treatment.
Venous Surgery
Surgery is a treatment option for more severe cases of varicose veins. Your doctor will discuss with you the various possible surgical procedures to help you decide which varicose vein treatment is best for you. One of the surgical methods is bandaging the veins and removing them through small incisions in the skin.

Venous surgery: before and after treatment
Vein ligation and removal is often successful in treating the symptoms and cosmetic problems of varicose veins. This operation is performed under local, spinal or general anesthesia in a hospital.
Complete recovery from this surgery usually takes about 2-4 weeks. Possible complications may include infection, bleeding, scarring, nerve damage, deep vein thrombosis, and adverse reactions to anesthesia.
Intravenous laser therapy
Intravenous laser therapy is a minimally invasive surgical procedure that involves laser radiation through a thin wire inserted into the affected vein, causing it to narrow.
Intravenous laser therapy has 98% of initial success. This procedure is performed on an outpatient basis under local anesthesia or light sedation.
Patients report less pain and faster healing with intravenous laser therapy than with ligation and removal of veins from surgery.
Radiofrequency ablation
Intravenous radiofrequency ablation is a minimally invasive procedure similar to intravenous laser therapy.
Instead of using laser light, a catheter inserted into a vein uses radio frequency energy, which heats and narrows the affected vessel.
As with intravenous laser therapy, patients report less pain and faster healing compared to venous ligation and removal.

Prevention of varicose veins
Although varicose veins are not always preventable, there are various methods you can take to reduce your chances of developing them.Prevention tips include:
- Regular exercise;
- Maintain a healthy weight;
- Avoid sitting or prolonged standing;
- Avoid squeezing your legs while sitting;
- Raise your legs higher when resting;
- Do not wear clothes that tighten your body around the waist, hips and legs.
Dear friends. This article is not medical advice and should not be used as a substitute for consulting a doctor.




































